Business overview
The Appeals and Grievances solution leverages stage-based case management capabilities of Pega Platform to manage benefit and payment related requests/complaints received from members and other interested parties (authorized representatives, providers, and third parties such as independent review entities). The solution supports three case types to manage and resolve complaints/requests: appeals, grievances, and organization determinations.
The following are the key features of the Appeals and Grievances solution:
- Stage-based case life cycle using the Pega Infinity Case Designer to manage the end-to-end Complaint process. Complaints are configured as case types with stages designed to describe each step in the process, beginning with the creation of the complaint and ending with the resolution and notification. The parent case type is Complaint. Within it, one can create one or more determination, appeal (reconsideration) and/or grievance subcases.
- Grievance Management Workflows – Start-to-end process for managing member grievances. This process includes the creation of a grievance case, capturing required information, such as incident date, grievance reason, and root cause of grievance. Based on user assigned urgency status (standard or expedited), system defines urgency and deadline and then routes the case to research/review for timely processing.
- Appeals Management Workflows – Start-to-end process for managing appeals filed for denial of service or claim payment. Capabilities include the creation of an appeal case, capturing relevant information, including information about the requestor party, appeal level, appeal category, service and or claim information, assigning an owner and standard or expedited urgency status, and applying appropriate service levels to ensure timely processing.
- Directed Web Access for External Users – A secure one-time link to the system sent to the provider who is the subject of a grievance to seek feedback on the issue when the grievance is related to providers or provider office staff (such as appointments, staff behavior, and prolonged wait times). After the provider submits the required information, the process automatically resumes and is routed to the owner of the case for review.
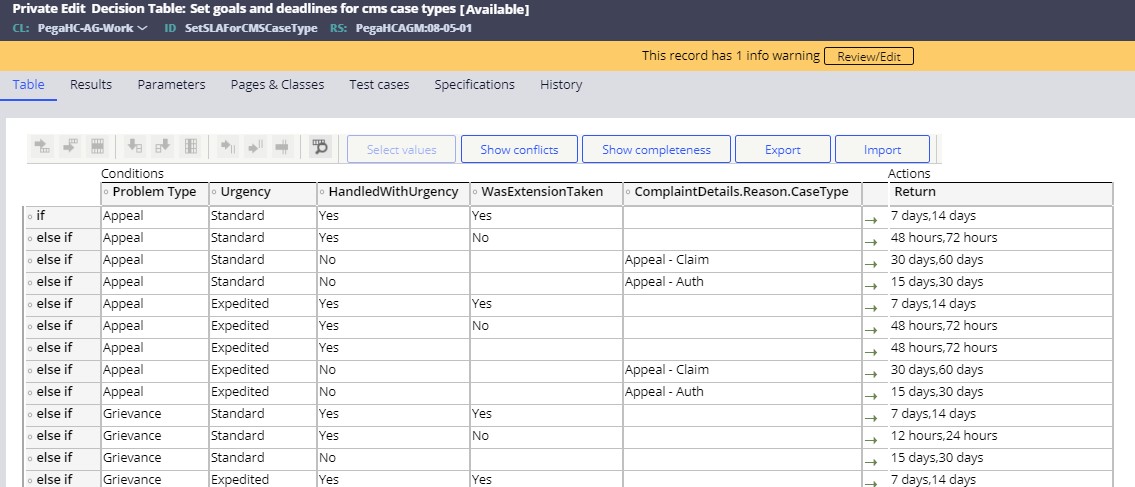
- Service Levels, Routing, Prioritization, and Escalation – Tracking of each
complaint case with priority assigned based on urgency status, type and level of
complaint, and type of denial. Service level rules monitor goal and deadline
times based on predefined standard parameters (14 days or 30 days). When the
case reaches goal times, additional priority points escalate the case relative
to other cases in the queue. Routing capabilities include requesting input from
supporting departments such as provider network services or utilization and
claims management. Service levels parameters (SLAs) may be configured to be
automatically driven by the member’s Line of Business (e.g., Commercial,
Medicare, Medicaid). The user configures the standard SLA parameters in the
following decision tables:
- SetSLAForCMSCaseType: This decision table drives SLAs for the following
out-of-the box Lines of Business (LOB): Medicare, Medicaid, and Federal
Program.
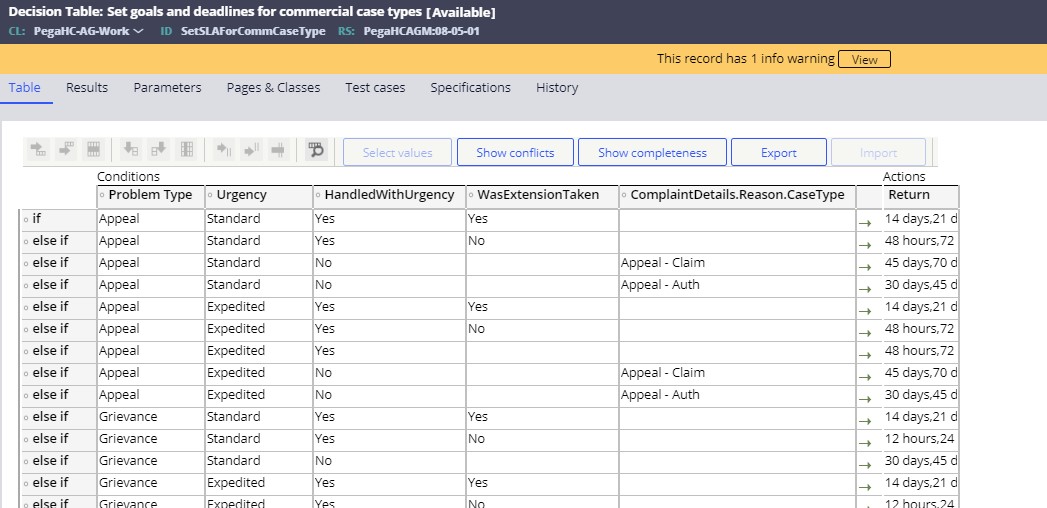
- SetSLAForCommCaseType: This decision table drives SLAs for the following
out-of-the box LOBs: Commercial, Behavioral Health, Individual, Consumer
Directed.
- SetSLAForCMSCaseType: This decision table drives SLAs for the following
out-of-the box Lines of Business (LOB): Medicare, Medicaid, and Federal
Program.
- Correspondence Generation – Preconfigured letter templates for communicating
with the involved parties at various stages of the complaint process. You can
quickly and easily customize standard templates for acknowledging a complaint,
requesting additional information, and communicating final disposition to meet
your specific needs. The letter templates are compiled dynamically and include
re-usable correspondence fragment rules for common sections such as headers,
footers, style sheets, and logos. You have the flexibility to generate
correspondence automatically in the background or to allow and require editing
as well as verification before it is finalized. Letter correspondence may be
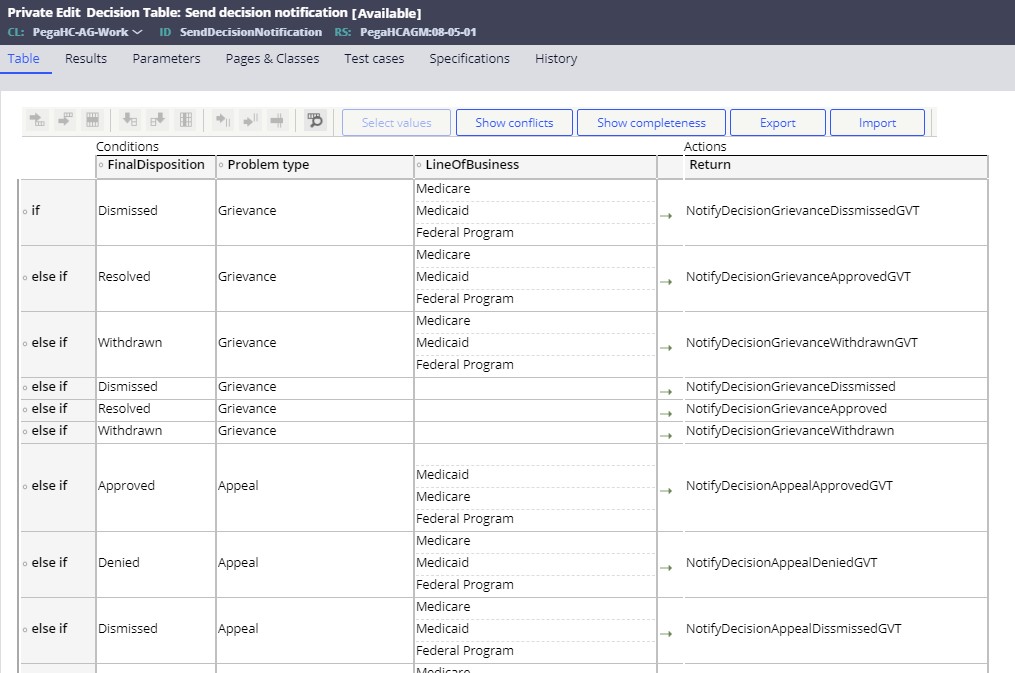
configured to be driven by the member’s Line of Business. Using the
SendDecisionNotification decision table, PFHC allows the user to configure the
automatic deployment of decision notification letter templates based on (a)
Problem type (grievance, appeal), (b) Disposition (dismissed, resolved,
withdrawn), and (c) Line of Business.
- Editing Letter Correspondence – The user may edit a single instance of letter correspondence prior to its deployment during the execution of the Resolve case step for Appeals and Grievances. When selecting Mail as the communication channel, the user has the option of clicking on the Edit correspondence link. In so doing, the system displays the letter that has been generated, allowing the user to edit both content and format before submitting the final version.
- Reports – The Appeals and Grievances Manager application includes a set of operational and administrative reports available out of box. Also, included in the report set are report definitions that support substantial compliance with CMS Part C Organization Determination Appeals and Grievances (ODAG) and Part D Coverage Determination Appeals and Grievances (CDAG) reporting requirements, including the capability to directly upload data in Excel output format.
This document is a consolidated use case document for Pega’s AGM solution. After complaint creation, user might have just an appeal or a grievance or a determination. This document covers appeal specific use cases, first followed by determination and then grievance uses cases. Use cases applicable to all three case types follow grievance related use cases.
Many organizations do not entertain expedited review of claims related to payment (payment disputes). Grievance expedited resolution is also not a general use case. By default, Pega AGM solution does not put any restriction on expedited review of case types.
- Complaint - Use-case (UC) 1: Create complaint
- Complaint - UC 2: Hold case for missing AOR
- Complaint - UC 3: Follow-up for AOR form
- Complaint - UC 4: Move case out of PendingAOR workbasket
- Appeal - UC 5: Review and research appeal information
- Appeal - UC 6: Clinical review of appeal information
- Appeal - UC 7: Perform medical review of an appeal
- Common - UC 8: Communicate appeals resolution
- Appeal - UC 9: Download appeal case packet
- Grievance - UC 10: Review and resolve grievance
- Grievance - UC 11: Request feedback from external users
- Determination - UC 12: Review and research determination case
- Determination - UC 13: Medical review of determination
- Determination - UC 14: Review and research Prescription Drug determination case
- Common - UC 15: Access case details/progress
- Common - UC 16: Universe and Operational reports
Previous topic Pega Foundation for Healthcare 8.7 Appeals and Grievances Manager Business Use Case Guide Next topic Complaint - Use-case (UC) 1: Create complaint
