System settings
System settings for the SCE are managed in two areas. The first is the SCE configuration page in the developer studio and the other is the System settings submenu in the configuration menu on the Business Analyst and Systems Manager portals.
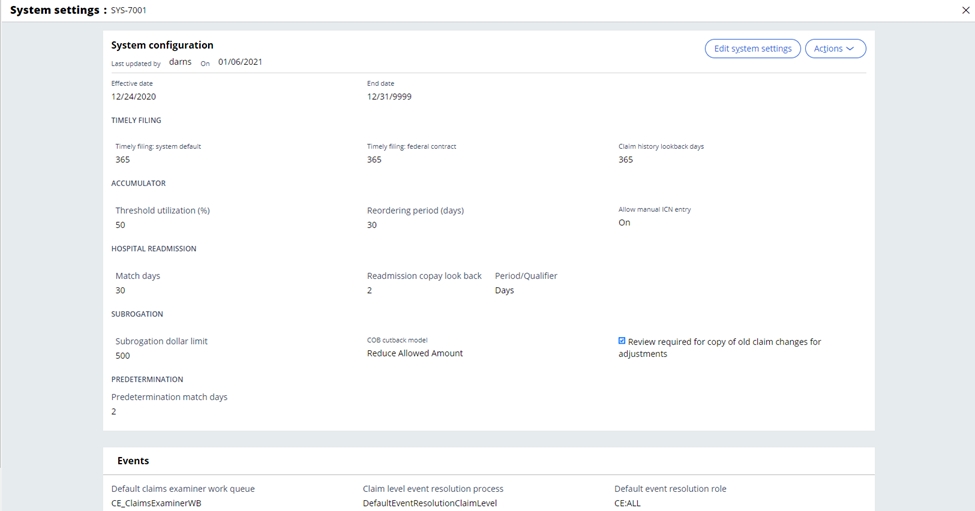
The system setting screen available on the portal provides a business analyst or systems manager with the capability to view and update key system configurations. Each configuration has an effective and end date and goes through the standard approval flow before the configuration is active. The system settings screen shows the last updated user and date in the banner. Audit and system settings history are available from the UX.
 System settings list
System settings listThe following table shows the list of fields in the system settings screen and the descriptions. More information on some of these settings will be detailed in the SCE capabilities where they are utilized.
Note: there must be an active system setting for the current processing date. If no active system setting is available, then event code SGB-0023 is applied to the claim.
| Section | Field | Description |
| System configuration | Effective date | Indicates the start date for the systems settings instance. |
| System configuration | End date | Indicates the expiration date for the systems settings instance. |
| System configuration | Timely filing: system default | Indicates the timely filing days limit for the timely filing event code should no other configuration exist. More information is available in the business edits section related to the timely filing event code. |
| System configuration | Timely filing: federal contract | Indicates the timely filing days limit configured for a federal contract. More information is available in the business edits section related to the timely filing event code. |
| System configuration | Retrieve claim history for the last (365) | Defines how many days to look back from the claim service from date when retrieving historical claims. This is used for gathering claims to be compared in the system audits (Duplicate Claim, Interim Bill processing, etc) and the adjustment/void/cancel processing. |
| System configuration | Accumulator: Threshold Utilization (%) | Defines the percentage of an authorization accumulator’s use that triggers a note to be routed to a workbasket for review. |
| System configuration | Allow manual ICN entry | This setting indicates whether an ICN may be manually entered by operators when entering the claim. In the instance an ICN is not entered, the SCE will automatically generate one. |
| System configuration | Hospital Readmission: Match Days | Defines the lookback period used to define a hospital readmission. More information is available in the business edits section detailing the hospital readmission functionality. |
| System configuration | Hospital Readmission: Readmission copay lookback | This setting is used to trigger the waiving of a copay for a hospital readmission. The period qualifier is expressed in Hours or Days. More information is available in the business edits section detailing the hospital readmission functionality. |
| System configuration | Subrogation: Subrogation dollar limit | This limit defines the minimum billed amount for a claim to be identified as a subrogation claim along with the other criteria. More information is available in the business edits section detailing the COB subrogation functionality. |
| System configuration | Subrogation: COB cutback model | Defines how COB payment information is used to calculate the final liability on claims in SCE. More information is available in the business edits section detailing the COB calculations. |
| System configuration | Review required for copy of old claim changes for adjustments | This setting is a yes/no setting which defines whether a claim that had previously been modified by an examiner needs to pend or ignore the updates when the provider submits an adjustment. If the setting is Yes, an adjustment submitted via EDI would automatically pend for review if the original claim was manually touched or corrected by a Claims Examiner. |
| System configuration | Predetermination: Predetermination match days | This setting defines the range (expressed in number of days) within which SCE matches a billable claim to a predetermination for dental services. |
| Events | Default claims examiner workbasket | Defines the workbasket used when the one defined for the event code configuration cannot be found or does not exist. |
| Events | Default system management workbasket | Defines the workbasket used when the one defined for the event code configuration cannot be found or does not exist. |
| Events | Claim level event resolution process | Defines the default resolution process used for event codes set at the claim level. |
| Events | Claim line level event resolution process | Defines the default resolution process used for event codes set at the claim line level. |
| Events | Default event resolution role | Defines the default role of the user assigned to event code resolution. |
| Events | Default end date | Defines the end date for system configurations where not otherwise defined. |
| Authorization | Minimum search results | This setting represents the minimum number of authorizations that will be returned when looking for a matching authorization. Along with the maximum search results setting, it defines the range of results to be returned. More information is available in the claim adjudication section on authorization processing. |
| Authorization | Automatic non exact authorization resolution | This setting defines whether the authorization should be utilized or an event code set, if the authorization is above the matching threshold, but does not match the claim information exactly. More information is available in the claim adjudication section on authorization processing. |
| Authorization | Authorization match days | Defines the period in which to search for authorizations (regardless of the status). All matched authorizations will be noted in the authorization history. More information is available in the claim adjudication section on authorization processing. |
| Authorization | Maximum search results | This setting represents the maximum number of authorizations that will be returned when looking for a matching authorization. Along with the minimum search results setting, it defines the range of results to be returned. More information is available in the section on authorization processing. |
| ClaimsXten | Allowed history claim lines | The setting allows users to define the maximum number of lines which would be sent to ClaimsXten. The maximum would include the current claim lines along with the historical claim lines for the member. More information is available in the section on ClaimsXten integration. |
| ClaimsXten | Send history | This indicator allows a user to configure if history needs to be sent to ClaimsXten in the request XML. More information is available in the section on ClaimsXten integration. |
| ClaimsXten | Send history, max lines exceeds | This setting defines whether to send the history or not when the number of history lines exceeds the allowed history count. More information is available in the section on ClaimsXten integration. |
| SLA | Default SLA | Defines the base SLA used in the urgency calculations. |
| SLA | Claim latency % | Defines the percentage of an SLA that has passed before the system triggers the latency action code |
| SLA | Organization name for SLA | Identifies who in the organization the SLA is configured for. This can be an internal department or external organization. This is used in event code configuration. |
| Manual pricing threshold | Pricing source reference | This setting allows the user to select the comparator (either non-par pricing table, or par pricing table) for limiting the allowed amount which can be entered manually during claim line re-pricing. |
| Manual pricing threshold | Threshold (%) | This setting allows the user to select the percentage of the existing price on the comparator as a threshold when manually pricing a claim line. |
| Security | Field level security configuration | This indicator determines whether field level security can be configured. |
| Benefits | Professional diagnosis for benefit determination | Identifies how many of the submitted diagnosis codes on a professional claim should be considered for benefit determination |
| Benefits | Dental diagnosis for benefit determination | Identifies how many of the submitted diagnosis codes on a dental claim should be considered for benefit determination |
| Reporting | Claim status not to be included | Defines the claim statuses which should not be included in the total number of claims processed report |
| Reporting | X12 Claim status to be included | Defines the claim statuses which should be included in the unprocessed claims report |
| Reporting | Adjudication claim status not to be included | Defines the claim statuses which should not be included in the average claim processing report |
| Policy selection and eligibility | Policy selection look back period (days) | When member search results are returned, the system retrieves all policies pertinent to the claim type (medical, dental) associated with the member record that fall within the Policy selection lookback period. The lookback is based on the earliest date of service on the claim. More information is available in the member match section. |
| Policy selection and eligibility | Policy eligibility start period (days) | This setting applies when the eligibility tie breaker is enabled. The system parses the "Service from" date on the claim and "looks back" the defined number of days for a policy with active eligibility. More information is available in the member match section. |
| Policy selection and eligibility | Policy eligibility end period (days) | This setting applies when the eligibility tie breaker is enabled. The system parses the "Service to" date on the claim and "looks forward" the defined number of days for a policy with active eligibility. More information is available in the member match section. |
| Policy selection and eligibility | Select policy category | If “Submitted policy” is enabled, SCE will adjudicate the claim against the policy submitted on the claim. If “Highest ranked policy” is enabled, the multiple policies are ranked by the SCE. More information is available in the member match section. |
| Member fuzzy search settings | Primary fuzzy search | Controls the application of the fuzziness defined in the fuzzy search configuration table. Turns the fuzziness On or Off for the primary fuzzy search. More information is available in the member match section. |
| Member fuzzy search settings | Secondary fuzzy search | Controls the application of the fuzziness defined in the fuzzy search configuration table. Turns the fuzziness On or Off for the secondary fuzzy search. More information is available in the member match section. |
| Newborn configuration settings | Newborn configuration | When set to "On", SCE will set an event code for all claims meeting the criteria on the newborn state-wise days configuration decision table. All claims for unenrolled newborns will be suspended without further attempt by SCE to determine the policy to process the claim against. More information is available in the member match section. |
| Member match tie breaker settings | Address tie breaker | When enabled, the address tiebreaker compares the submitted member address to the address in the system of record. If a match is found, the member record is selected for adjudication. This tiebreaker, if enabled, is only applied if SCE cannot determine which member record to select when there are multiple matches. More information is available in the member match section. |
| Member match tie breaker settings | Eligibility tie breaker | When enabled, the eligibility tiebreaker compares the earliest date of service on the claim to the eligibility spans of the matching member records. If a single active policy is found, SCE will select the member associated with that policy for adjudication. This tiebreaker, if enabled, is only applied if SCE cannot determine which member record to select when there are multiple matches. More information is available in the member match section. |
| Transplant configuration | Transplant claims configuration | When set to "On", SCE will set an event code for all claims submitted with an individual relationship code of 39 or 40. All claims for transplant donors will be suspended without further attempt by SCE to determine the policy to process the claim against. More information is available in the member match section. |
| Standalone member search settings | Member search results limit | This limits the number of search results returned when a member search is performed. More information is available in the member match section. |
| Standalone member search settings | Member search look back period | Defines the lookback period (in days) for member policies returned as part of the search results. More information is available in the member match section. |
| Member notification setting | Generate system notification | When a no member found or multiple members found event code is raised on a claim and a member is selected by the claims examiner, users can choose to have SCE create a system notification. More information is available in the member match section. |
To update the system settings, select the Edit system settings button on the System configuration screen. The System configuration screen will then be editable for the user to make any appropriate changes. Once changes have been made, select the Done Editing button. Once the system settings are valid and are configured to be effective today, or a date in the future, comments for the approver have been made, the changes can be submitted for approval by selecting Submit. Once the changes have been submitted, the user will be notified that the requested settings have been sent for approval, along with the task ID. At any time during the editing, the user can discard the changes, but selecting the Discard button and return to the previous version.
Key items to consider when making system configuration changes:
- Smart Claims Engine allows the user to create and store system settings instances that have a future effective date. In this situation, the current settings remain in effect until the user-defined start date of the new instance.
- When the user creates a new system setting instance that will become effective in the future, Smart Claims Engine automatically changes the end date of the current instance to the day prior to the start date of the future instance.
- All future system settings are displayed in the audit history in chronological order with the most current instance on top.
- SCE will display a validation error if the system settings are configured for a past date.
- Smart Claims Engine also ensures that system settings run concurrently and, therefore, does not allow gaps in system settings, or overlapping dates. A validation error is displayed if a configuration has been created with a gap.
Both the history of each individual system setting instance, and the history of all system configuration changes in Smart Claims Engine may be viewed from the System configuration screen by clicking on the Actions button in the top right-hand corner and then selecting the desired view.
When the user selects Setting instances, a text box is displayed showing, in list form, all previous (and future scheduled) system setting instances, including a unique ID number for each individual setting, effective and end dates, and other key data.
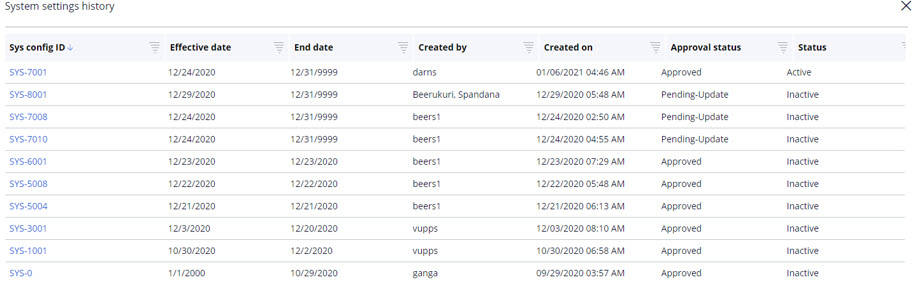
Selecting the Sys config ID in this screen will show the full view of the corresponding system configuration page in read-only mode.
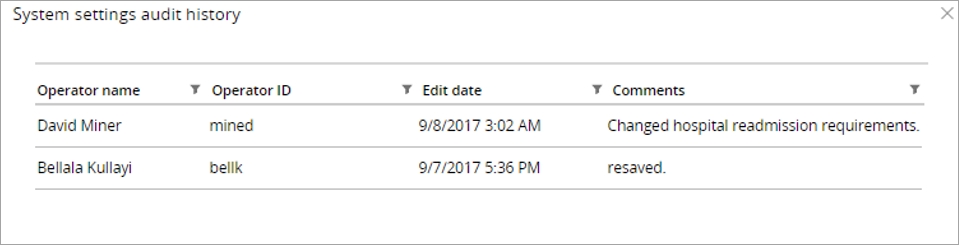
When the user selects the Audit history, a text box is displayed that includes in list form all changes to the individual setting instance, including operator name and ID, edit date, and any comments that were associated to the changes.
Dev studio SCE configuration settings
The SCE provides some configurations in the dev studio. To access these configuration settings, select the Claims Engine Configuration from the Claims Engine item on the Configure menu.
Top portion of the configuration screenThe top portion of this tab describes the major settings for the
configuration of this application. 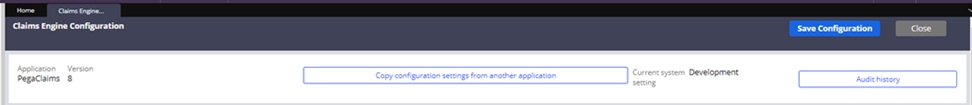
| Field | Description |
| Application | Shows the current version of the Pega Claims application. |
| Copy configuration settings from another application | Enables the configuration settings to be copied from another layer in the application stack. |
| Current system setting | Displays the Data-Admin-System setting value that characterizes the need for access security on this system. Available values are: Production (5) Pre-Production (4) Test (3) Development (2) Experimental (1) You can use this value to influence processing based on the use of the system, for example, Production versus Test. |
| Audit history | Displays the audit history and associated comments for the configuration screen. |
Application configuration tab
The application configuration tab contains many of the application level settings. These global level settings define how the claim is processed and are required by the application.
| Section | Field | Description |
| Module setting | Global measurement | Indicates whether the timing of all modules should be captured. When this is off, the individual module timing configuration can be enabled. |
| Module setting | Global audit messages | Indicates whether the audit messages of all modules should be captured. When this is off, the individual module audit configuration can be enabled. |
| Subscriber lock settings | Subscriber lock | An indicator that defines whether to use the Subscriber Lock feature in the application. If On, the Subscriber Lock feature is activated, which means that you cannot process any subsequent claims for a specific subscriber until the lock is released. Claims for that subscriber are pended until the lock is released. If Off, the Subscriber Lock feature is deactivated, which means that claims you are processing are not subject to subscriber locking. Subscriber locking prevents concurrent claims for the same subscriber being processed, impacting accumulator calculations and duplicate checking. |
| Subscriber lock settings | Subscriber lock recycle interval | The time when claims that have set the subscriber lock are resubmitted for processing. |
| Split claim settings | Split claim | The radio button enables or disables the manual splitting of claims. |
| Split claim settings | Manual split claim threshold | Manual split claim threshold defines the maximum number of new claims that may be created when manually splitting a claim. |
| Configuration settings | Config applies to | Defines the class that this application references when resolving custom rules. |
| Configuration settings | Configuration work class | Defines the class to which claims processed by this application instance are saved. |
| Configuration settings | Configuration history class | Defines the class to which the history for claims processed by this application instance is saved. |
| Configuration settings | Reprocess count | Defines the value for how many times the claim can go through reprocessing. |
| Event settings | Use client event code | Using the client event code option will allow the client’s event codes IDs to displayed in the event code list. |
| Event settings | Event code reporting interval | Defines the interval used to report event process times. |
| Event settings | Event code implementation ID order of resolution | Defines the order of event codes to be processed in the SCE by their implementation ID. To modify, select the Modify event code implementation ID button. |
| Claim processing settings | Process claims status list | This list defines the claims status that are processed through the new claims job scheduler. The default is just new claims, but other statuses can be added by selecting the Modify status list button. Note: this is only displayed when queue processors are switched off via the dynamic system setting: EnableQPForClaimProcessing = false |
| Claim processing settings | Process Pending-Reprocess claims every | The Pending-Reprocess claims can run every minute, hour, day, or week based on the setting. These claims can also be processed immediately by pressing the Process now button. Note: this is only displayed when queue processors are switched off via the dynamic system setting: EnableQPForClaimProcessing = false |
| Claim processing settings | Process new claims every | The new claims process can run every minute, hour, day or week based on the setting. New claims can also be processed immediately by pressing the Process now button. Note: this is only displayed when queue processors are switched off via the dynamic system setting: EnableQPForClaimProcessing = false |
| Claim processing settings | Process recycle claims | The Process now button can be used to immediately process any claims that are in Process-Recycle status |
| Claim processing settings | Initiate 835 process | The Initiate 835 Process would generate an 835 file selecting claims which were not selected on the previous 835 generation run. |
| Claim processing settings | Available claim identifiers | Allows the user to modify current claim identifiers to support system configurations (All, Chargeable, Medicaid Reclamation, Reporting). |
| Claim processing settings | Resolution flows | List of available resolution flows to support event code disposition configuration. To modify, select the Modify resolution flows list button. |
| Claim processing settings | Create claim WO from EDI batch transactions | Selecting the Process now button will create the claims from any EDI batch transactions that have been parsed. |
This section enables the creation and management of modules, sequences and orchestrations that support the processing of claims. More information is found in the section on Modules, sequences, and orchestrations in this section.
Claim edits tabThe claim edits tab controls the key information needed for specific claim types, as well as the configurations for the duplicate claim rules. The duplicate claim rules are detailed in the section for duplicate claim edits. This section will cover the key fields used to configure claim types in the system.
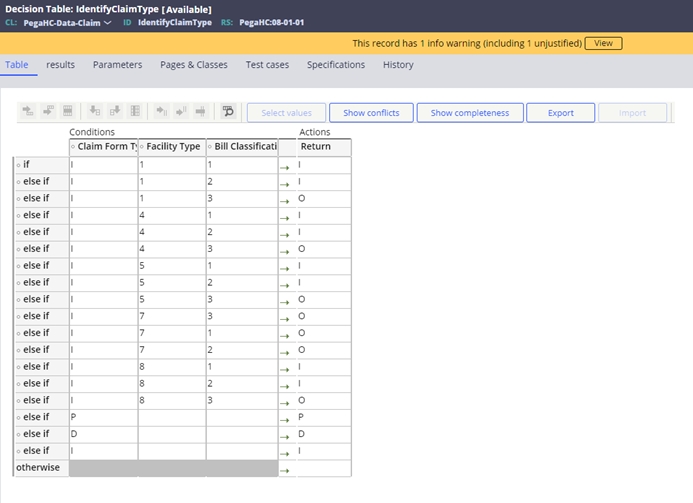
The claim type is defined based on a series of parameters. The Claim Type Identification link below the parameters displays the configuration for the claim type. The Type indicates the form type (Institutional, Professional, Pharmacy and Dental). The facility type and bill classification come from the fields on the institutional form to classify institutional claims into different claim types. Changes may be made to the configuration on the IdentifyClaimType decision table.
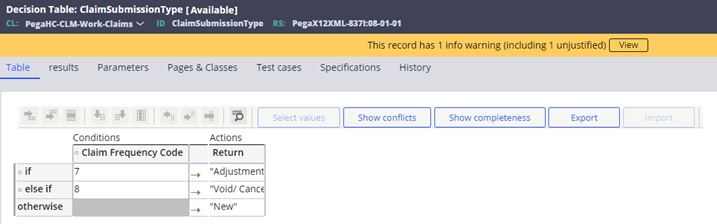
The claim transaction type is also broken down into three types based on the claim frequency code. You can access this table through the Claim Submission Type Mapping link on the Claim Edits tab. Changes may be made to the configuration on the ClaimSubmissionType decision table.
To configure the system to support on un-support the specific claim type, you can select +Add item, or X Delete. You can also copy an existing claim type configuration by selecting Copy claim type. To edit an existing type, double click on the claim type to be modified.
| Field | Description |
| Claim type | The type of claim this configuration is for. If a claim is received and maps to an unconfigured type through the IdentifyClaimType decision table, SVE-0024 will set. |
| Claim Billing | Indicates whether claims are processed for billing purposes. (claim identifier CH). If this identifier is not configured in the system, a claim possessing it will set SVE-0013. |
| Claim Reporting | Indicates whether claims are processed for reporting purposes. (claim identifier RP). If this identifier is not configured in the system, a claim processing it will set SVE-0013. |
| Claim Subrogation | Indicates whether claims are processed for Medicaid subrogation purposes (claim identifier 31). If this identifier is not configured in the system, a claim possessing it will set SVE-0013. |
| Processing Level | If the processing level is Header, the payment is made at the claim level once all claim lines (Detail) have been completed and approved. If the processing level is Detail, payment is made at the claim line level as it is completed and approved. If the processing level is not configured, SVE-0010 will set on the claim. |
Each claim identifier selected for processing will create a separate configuration for the history retrieval, the claim submission types and the duplicate edit configuration.
History retrieval – This allows the system to consider multiple claim types when retrieving history for the purposes of system audits. Clicking on a claim type will add it to the selected section. Clicking it in the selected section will remove it from consideration.
Duplicate Claim Edits – This provides the ability to select the fields and appropriate weights for exact and suspect duplicate edits. More information can be found in the section on Duplicate Edit section of Business edits.
Submission type – This defines the submission types that can be processed for this claim type and claim identifier. If a submission type is not configured and a claim meeting that criteria as defined in the ClaimSubmissionType decision table, SVE-0011 will be set.
The configuration settings can be changed easily in the developer studio. Once the changes have been performed, press Save Configuration, enter comments in the popup box and press Submit. Selecting Cancel will return to the configuration screen. Selecting Close on the main screen will close the configuration screen without saving the changes.
Previous topic Core configurations Next topic Event code management
