Field labels
This section defines the fields on the claim screen user interface. The fields within each core section outlined below are identified and defined; note that some fields are accessed via hyperlink.
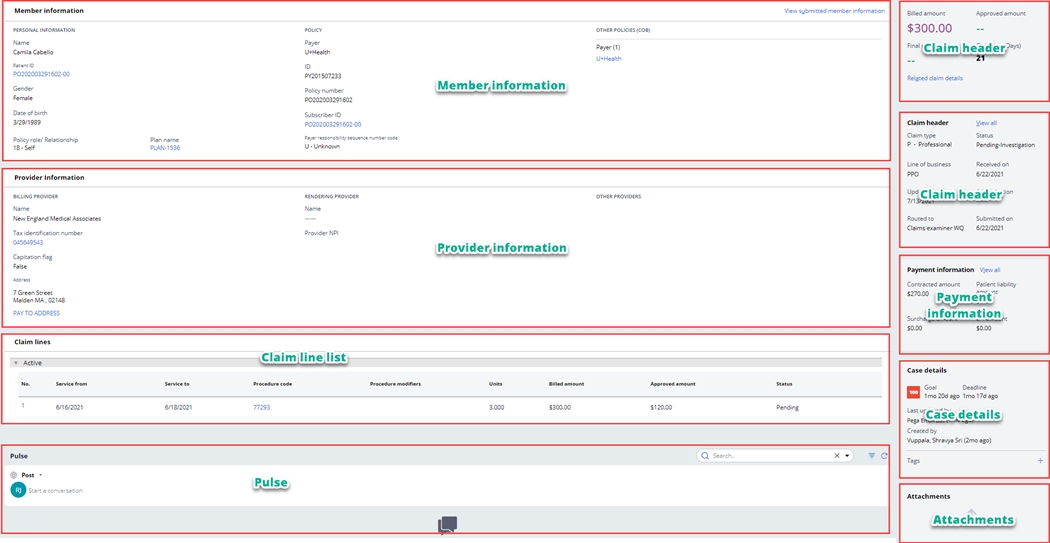
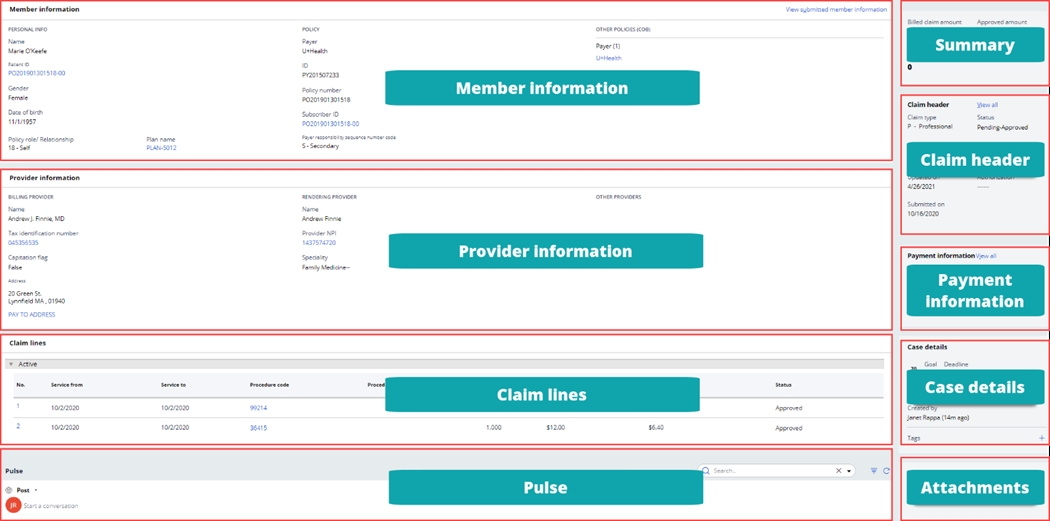
Unless otherwise noted, each field in the list appears on all claim types.
| Section | Field name | Description |
| Member information | View submitted member information | The View submitted member information hyperlink opens the Submitted member information pop up, displaying the subscriber and patient information as it was submitted on the claim. Note: when only subscriber information is submitted, only subscriber information is displayed. |
| Member information | Name | The matched patient's first and last name. |
| Member information | Patient ID | The patient’s identification number for the matched policy. The Patient ID hyperlink opens the Member details pop up. |
| Member information | Gender | The matched patient's gender. |
| Member information | Date of birth | The date of birth of the matched patient. |
| Member information | Policy role/relationship | The matched patient’s relationship to the subscriber. |
| Member information | Plan name | The matched plan name. The Plan name hyperlink provides access to details from PHFC regarding the patient's plan. |
| Member information | Payer | The name of the payer. |
| Member information | ID | The identification number of the payer. |
| Member information | Policy number | The member's policy number. |
| Member information | Subscriber ID | The identification number of the subscriber. The Subscriber ID hyperlink opens the Member details pop up. |
| Member information | Payer responsibility sequence number code | The policy’s order of responsibility for adjudicating the claim. |
| Submitted member information pop up | ID | The identification number of the subscriber as submitted on the claim. |
| Submitted member information pop up | Date of birth | The subscriber's date of birth as submitted on the claim. |
| Submitted member information pop up | Name | The subscriber's first name, middle initial, and last name as submitted on the claim. |
| Submitted member information pop up | Address | The subscriber's address as submitted on the claim. |
| Submitted member information pop up | Gender | The subscriber's gender as submitted on the claim. |
| Submitted member information pop up | Policy role/relationship | The subscriber's relationship code as submitted on the claim. |
| Submitted member information pop up | ID | The identification number of the patient as submitted on the claim. |
| Submitted member information pop up | Date of birth | The patient's date of birth as submitted on the claim. |
| Submitted member information pop up | Name | The patient's first name, middle initial, and last name as submitted on the claim. |
| Submitted member information pop up | Address | The patient's address as submitted on the claim. |
| Submitted member information pop up | Gender | The patient's gender as submitted on the claim. |
| Submitted member information pop up | Policy role/relationship | The patient's relationship code as submitted on the claim. |
| Member details pop up | Master ID | The master identification number associated to the patient. |
| Member details pop up | First name | The patient's first name. |
| Member details pop up | Middle name | The patient's middle name. |
| Member details pop up | Last name | The patient's last name. |
| Member details pop up | Suffix | The patient's suffix. |
| Member details pop up | Address line 1 | The first line of the patient's address. |
| Member details pop up | Address line 2 | The second line of the patient's address. |
| Member details pop up | City | The patient's city of residence. |
| Member details pop up | State | The patient's state of residence. |
| Member details pop up | Zip code | The patient's zip code. |
| Member details pop up | Gender | The patient's gender. |
| Member details pop up | Date of birth | The patient's date of birth. |
| Member details pop up | Category | Indicates the type of policy - medical, dental, etc. |
| Member details pop up | ID | The patient's identification number for the policy. |
| Member details pop up | Effective date | The effective date of the policy. |
| Member details pop up | End date | The end date of the policy. |
| Member details pop up | Identifier | The identification number for the policy type. |
| Member details pop up | Type | The type of policy. |
| Member details pop up | Name | The name of the patient's primary care provider. Displayed only if member has a PCP on record. |
| Member details pop up | Specialty | The specialty of the patient's primary care provider. Displayed only if member has a PCP on record. |
| Member details pop up | Effective date | The effective date of the patient's primary care provider relationship. Displayed only if member has a PCP on record. |
| Member details pop up | End date | The end date of the patient's primary care provider relationship. Displayed only if member has a PCP on record. |
| OTHER POLICIES (COB) | Payer | The name of the other payer(s) for the member |
| OTHER POLICIES (COB) | Other subscriber ID | The identification number of the other insurance subscriber. |
| OTHER POLICIES (COB) | Last name/organization name | The last name or organization name of the other insurance subscriber. |
| OTHER POLICIES (COB) | Individual relationship code | The other insurance subscriber's individual relationship code. |
| OTHER POLICIES (COB) | Address | The other subscriber's address. |
| OTHER POLICIES (COB) | Benefit assignment certification indicator | The benefit assignment certification indicator of the other subscriber. |
| OTHER POLICIES (COB) | Release of information | The release of information indicator for the other subscriber. |
| OTHER POLICIES (COB) | Other payer ID | The identifier for the other insurance payer. |
| OTHER POLICIES (COB) | Other payer organization name | The name of the other insurance payer. |
| OTHER POLICIES (COB) | Claim control number | The claim number associated with the other insurance payment. |
| OTHER POLICIES (COB) | Payer responsibility sequence number | The other insurance policy’s order of responsibility for adjudicating the claim. |
| OTHER POLICIES (COB) | Address | The address of the other insurance payer. |
| OTHER POLICIES (COB) | Paid amount | The total paid amount the other payer paid for the claim. |
| OTHER POLICIES (COB) | Paid date | The date the other payer paid the claim. |
| OTHER POLICIES (COB) | Patient's remaining liability | The remaining patient liability after the other payer paid the claim. |
| OTHER POLICIES (COB) | Non covered amount | The amount not covered when the other payer paid the claim. |
| OTHER POLICIES (COB) | Check number | The check number associated with the other payer's claim payment. |
| OTHER POLICIES (COB) | Adjustment group code | The adjustment group code used by the other payer to indicate liability for non-paid amounts on the claim. |
| OTHER POLICIES (COB) | Reason code | The reason code used by the other payer to explain non-paid amounts on the claim. |
| OTHER POLICIES (COB) | Description | The description associated with the reason code used by the other payer to explain non-paid amounts on the claim. |
| OTHER POLICIES (COB) | Amount | The dollar amount of the adjustment. |
| OTHER POLICIES (COB) | Quantity | The quantity of the adjustment. |
| Section | Field name | Description |
| BILLING PROVIDER | Name | The name of the billing provider. |
| BILLING PROVIDER | Tax identification number | The billing provider's tax identification number. The Tax identification number hyperlink leads to detailed billing provider information. |
| BILLING PROVIDER | Capitation flag | The capitation flag indicates whether the provider is subject to a capitation agreement. |
| BILLING PROVIDER | Address | The full address of the billing provider. |
| BILLING PROVIDER | PAY TO ADDRESS | The pay to address of the billing provider. The Pay to address hyperlink opens a pop up displaying the address entered. |
| RENDERING PROVIDER | Name | The name of the rendering provider. |
| RENDERING PROVIDER | Provider NPI | The rendering provider's National Provider Identifier (NPI). The Provider NPI hyperlink leads to detailed rendering provider information. |
| RENDERING PROVIDER | Specialty | The specialty of the rendering provider. |
| OTHER PROVIDERS | Provider type | When provider types other than billing and rendering are submitted on the claim, SCE displays the provider type (for example, operating provider or service facility) above a hyperlink that leads to detailed information about the other provider(s). |
| Section | Field name | Description |
| Claim lines | No. | The claim line number. |
| Claim lines | Service from | Professional, outpatient, and inpatient claims only - The Service from date indicates the starting month, day, and year the service(s) was provided. |
| Claim lines | Service to | Professional, outpatient, and inpatient claims only - The Service to date indicates the ending month, day, and year the service(s) was provided. |
| Claim lines | Procedure date | Dental claims only - The procedure date indicates the starting month, day, and year the service(s) was provided. |
| Claim lines | Procedure code | Professional and dental claims only - The procedure code identifies the medical services and procedures provided to the patient. |
| Claim lines | Procedure modifiers | Professional claims only - The procedure code modifier provides supplemental information for the procedure code billed. |
| Claim lines | Area of oral cavity | Dental claims only - The area of oral cavity is a code which reports what part of the mouth the procedure billed on the claim line applies to. |
| Claim lines | Tooth surface | Dental claims only - The tooth surface is a code which reports which part of the tooth the procedure billed on the claim line applies to. |
| Claim lines | Units | Professional, outpatient, and inpatient claims only - The units field captures the count of the services reported on the claim line. |
| Claim lines | Billed amount | The billed amount indicates the total charged by the provider for the claim line. |
| Claim lines | Approved amount | The approved amount is the amount due to the payee for all the services on the claim. |
| Claim lines | Status | The adjudication status of the claim line. |
| Claim lines | Revenue code | Outpatient and inpatient claims only - The revenue code is used to identify specific accommodations and/or ancillary charges. |
| Claim line details | Service from | The Service from date indicates the starting month, day, and year the service(s) was provided. |
| Claim line details | Service to | The Service to date indicates the ending month, day, and year the service(s) was provided. |
| Claim line details | Treatment start date | Dental claims only - The beginning date of treatment for the service billed on the claim line. |
| Claim line details | Treatment completion date | Dental claims only - The end date of treatment for the service billed on the claim line. |
| Claim line details | Orthodontic banding date | Dental claims only - The date orthodontic banding was performed. |
| Claim line details | Replacement date | Dental claims only - The date the appliance or prosthesis was replaced. |
| Claim line details | Predetermination of benefits identifier | Dental claims only - The identification or reference number of the predetermination of benefits submission. |
| Claim line details | Adj repriced line reference number | Dental claims only - The line number of an adjusted repriced line item adjusted from an original amount. |
| Claim line details | Prosthesis crown or inlay code | Dental claims only - The code specifying the placement status for the dental work. |
| Claim line details | Prior placement date | Dental claims only - The date of the prior placement of the prosthesis, crown, or inlay. |
| Claim line details | Place of service | For professional and dental claims only - The place of service code and description submitted on the claim line. |
| Claim line details | Oral cavity designation code | Dental claims only - The oral cavity designation code indicates the area of the oral cavity associated with the service submitted on the claim line. |
| Claim line details | Tooth code | Dental claims only - The tooth code indicates the tooth associated with the service submitted on the claim line. |
| Claim line details | Tooth surface code | Dental claims only - The tooth surface code indicates the part of the tooth associated with the service submitted on the claim line. |
| Claim line details | Revenue code | Outpatient and inpatient claims only - The revenue code is used to identify specific accommodations and/or ancillary charges. |
| Claim line details | National drug code | Professional, outpatient, and inpatient claims only - The National Drug Code (NDC) is a unique, three-segment number which serves as an identifier for drugs. |
| Claim line details | Procedure code | The procedure code identifies the medical services and procedures provided to the patient. |
| Claim line details | Procedure code qualifier | Outpatient and inpatient claims only - Identifies an additional attribute of the procedure reported. |
| Claim line details | Unit qualifier | The units qualifier further describes the units billed, denoting, days, units, etc. |
| Claim line details | Procedure modifiers | The procedure code modifier provides supplemental information for the procedure code billed. |
| Claim line details | Service unit | Outpatient and inpatient claims only - The service unit field captures the count of the services reported on the claim line. |
| Claim line details | Non covered charges | Outpatient and inpatient claims only - Non-covered charges for the claim service line as submitted by the provider. |
| Claim line details | Claim approved units | The number of units approved for payment on the claim service line. |
| Claim line details | Benefit | The benefit matched to the claim line based on the service, diagnosis and other factors billed on the claim. |
| Claim line details | Prior authorization | The prior authorization number, referral number, mammography pre-certification number, or Clinical Laboratory Improvement Amendments (CLIA) number, as assigned by the payer for the current service. |
| Claim line details | Adjudicated authorization | The actual prior authorization number, referral number, mammography pre-certification number, or Clinical Laboratory Improvement Amendments (CLIA) number applied during claim adjudication. |
| Claim line details | PROVIDERS | When claim line level providers are reported, SCE displays the provider type (for example, operating provider or service facility) above a hyperlink that leads to detailed information about the other provider(s). |
| Claim line details | Unit of service | For professional and dental claims only - The unit of service field captures the count of the services reported on the claim line. |
| Execution result | Billed amount | Billed amount represents the charge for the claim line service submitted on the claim by the provider. |
| Execution result | Approved amount | The approved amount is the amount due to the payee for the services billed on the claim line. |
| Execution result | Status | The adjudication status of the claim line. |
| Execution result | Contracted amount | The initial maximum dollar amount a payer would pay for a given service line on the claim. |
| Execution result | Allowed amount | The final amount payable for the claim line. Factors such as surcharge amount and billed amount (when lesser than the allowed amount) are taken into consideration. |
| Execution result | Surcharge amount | The surcharge amount applicable to the claim line. |
| Execution result | GME % | The percentage applied for the graduate medical expense surcharge. |
| Execution result | Pricing source | The source for the price applied to the claim service line. |
| Execution result | Pricing method | The method for calculating the price applied to the claim service line. |
| Deductible amount | The deductible amount due from the member for the services on the claim line. | |
| Coinsurance amount | The coinsurance amount due from the member for the services on the claim line. | |
| Execution result | Member penalty amount | The amount of any penalty applied to the member. |
| Copay | The copay amount due from the member for the services on the claim line. | |
| Execution result | Additional liability amount | Captures any additional member liability for the services billed on the claim line |
| Execution result | Copay calculation method | Indicates how the copay is calculated by the benefit plan. |
| Execution result | Finalized paid date | The date the check/EFT was issued by the payer. |
| Check or EFT number | The check or Electronic Funds Transfer (EFT) number associated with the payment. | |
| Execution result | Adjudication date | The date the adjudication of the claim line was completed. |
| Execution result | Network ID | The identifier for the network matched to drive payment calculations. |
| Execution result | Total patient liability amount | The total patient liability for the services submitted on the claim line. |
| Execution result | Non-covered patient liability amount | The patient liability for non-covered services submitted on the claim line. |
| Execution result | Final paid amount | The amount paid for services submitted on the claim line. |
| Execution result | Capitation flag for API | An indicator for capitation. |
| Execution result | Ratesheet ID | The identifier for the provider ratesheet. |
| Execution result | DOFR indicator | Indicates that the claim line is subject to a Division of Financial Responsibility (DOFR) provision. |
| Execution result | Participating network | The indicator of whether the provider is participating or non-participating. |
| Execution result | Contract ID | The provider's contract identifier. |
| Execution result | Info from external system | The Info from external system hyperlink provides access to information from external systems (for example, ClaimsXten or NetworX Pricer) used in the claim line adjudication. |
| Execution result | Pricing Sources | The Pricing Sources hyperlink provides access to the pricing sources, methodologies, and dollar amounts generated during claim line adjudication. |
| Adjustment details | Other payer | The other insurance payer identifier for other insurance payments associated to the claim line. This field is expandable for access to details regarding the adjustment group code, reason code, description, amount, and quantity associated with the claim line. |
| Adjustment details | Paid amount | The amount paid by the other insurance payer for the claim line. |
| Adjustment details | Remaining patient liability | The remaining patient liability amount for the claim line after adjudication by the other payer. |
| Adjustment details | Paid service unit count | The service unit count of services paid on the claim line by the other payer. |
| Adjustment details | Procedure code | The procedure code submitted by the other insurance payer for the claim line. |
| Adjustment details | Adjustment group code | The adjustment group code used to indicate liability for non-paid amounts on the claim line. |
| Adjustment details | Reason code | The reason code used to explain non-paid amounts on the claim line. |
| Adjustment details | Description | The description associated with the reason code used to explain non-paid amounts on the claim line. |
| Adjustment details | Amount | The amount of the claim line adjustment. |
| Adjustment details | Quantity | The quantity associated with the claim line adjustment. |
| Adjustment details | Remittance advice remark code | The code used to further explain the adjustment to the claim line. |
| Adjustment details | Description | The description associated with the code used to further explain the adjustment to the claim line. |
Pulse provides the ability for you to post messages and receive replies.
Summary section| Section | Field name | Description |
| Summary | Billed amount | The billed amount indicates the total charged by the provider for all the services on the claim. |
| Summary | Approved amount | The approved amount is the amount due to the payee for all the services on the claim. |
| Summary | Final paid amount | The amount paid by the payer to the payee for all the services on the claim. |
| Summary | Claim age (Days) | The age of the claim calculated based on the submitted date of the claim. |
| Summary | Related claim details | The Related claim details hyperlink appears when there are automatically or manually related claims. |
| Section | Field nameField name | Description | |
| Claim headerClaim header | Claim type | The claim type of the claim. | |
| Claim headerClaim header | Status | The current adjudication status of the claim. | |
| Claim headerClaim header | Line of business | The line of business associated with the policy. | |
| Claim headerClaim header | Received on | The date the claim was received by the EDI gateway. | |
| Claim headerClaim header | Updated on | The date of the most recent update to the claim. | |
| Claim headerClaim header | Routed to | Displayed on unresolved claims only, the routed to field indicates the work queue or work list to which the claim is routed. | |
| Claim headerClaim header | Authorization | The authorization submitted by the provider at the claim header level. | |
| Claim headerClaim header | Submitted on | The date the claim was submitted into the SCE. | |
| Claim headerClaim header | Tooth numbers/letters | Dental claims only - The Tooth numbers/letters chart indicates missing teeth and/or teeth to be extracted. You can choose to view a maxillary or mandibular tooth chart. | |
| Claim informationClaim information | Service date from-to | Professional and dental claims only - The date span of the services submitted on the claim. | |
| Claim informationClaim information | Place of service | Professional and dental claims only - The claim level place of service code and description. | |
| Claim informationClaim information | Accident type | Professional and dental claims only - The type of accident associated with the services rendered on the claim. | |
| Claim informationClaim information | Accident country | Professional and dental claims only - The country where the accident associated with the services rendered on the claim occurred. | |
| Claim informationClaim information | Accident state | Professional and dental claims only - The state where the accident associated with the services rendered on the claim occurred. | |
| Claim informationClaim information | Date of accident | Professional and dental claims only - The date the accident associated with the services rendered on the claim occurred. | |
| Claim informationClaim information | Other insurance indicator | Professional and dental claims only - Indicates whether other insurance coverage for the accident exists. | |
| Claim informationClaim information | Claim referral number | Professional and dental claims only - The referral number associated with the services rendered on the claim. | |
| Claim informationClaim information | ICN | Dental claims only - The internal control number for the claim. | |
| Claim informationClaim information | Submitter claim number | Professional, outpatient, and inpatient claims only - The claim number provided by the submitter of the claim. | |
| Claim informationClaim information | Claim identifier | The claim identifier for the claim. | |
| Claim informationClaim information | Transaction type | The transaction type for the claim. | |
| Claim informationClaim information | Media type | Professional and dental claims only - The media type of the claim submission. | |
| Claim informationClaim information | Capitation flag | Indicates whether the claim was processed as capitated. | |
| Claim informationClaim information | Line of business | The line of business associated with the policy. | |
| Claim informationClaim information | Info from external system | The Info from external system hyperlink provides access to information from external systems (for example, ClaimsXten, NetworX Pricer or another adjudication system) that may have been used in the claim adjudication. | |
| Claim informationClaim information | Object ID | The work object identifier for the claim work object. | |
| Claim informationClaim information | Diagnosis type | The type of diagnosis submitted for the claim. | |
| Claim informationClaim information | Principal diagnosis code | The principal diagnosis related to the services submitted on the claim. | |
| Claim informationClaim information | Present on admission | An indicator of whether the diagnosis was present upon the patient's hospital admission date. | |
| Claim informationClaim information | Other diagnosis codes | Professional and dental claims only - Additional diagnosis codes associated with the patient. | |
| Claim informationClaim information | Is predetermination of benefits | Dental claims only - Indicates whether the submitted claim is for predetermination of benefits. | |
| Claim informationClaim information | Prior authorization number | Outpatient, inpatient, and dental claims only - The prior authorization number assigned by the payer for the current service. | |
| Claim informationClaim information | Predetermination of benefits identifier | Dental claims only - The identification or reference number of the predetermination of benefits submission. | |
| Claim informationClaim information | Is treatment for orthodontics | Dental claims only - Indicates whether services billed were for orthodontic treatment. | |
| Section | Field name | Description |
| Payment information | Contracted amount | The initial maximum dollar amount a payer would pay for all service lines on the claim. |
| Payment information | Patient liability amount | The total patient liability for the services submitted on the claim. |
| Payment information | Surcharge amount | The total dollar amount of any surcharges applied to the claim. |
| Payment information | LPI amount | The total late payment interest amount paid for the claim. |
| Payment details | Billed amount | The billed claim amount indicates the total charged by the provider for all the services on the claim. |
| Payment details | Approved amount | The approved amount is the amount due to the payee for all the services on the claim. |
| Payment details | Status | The overall claim status. |
| Payment details | Contracted amount | The initial maximum dollar amount a payer would pay for all service lines on the claim. |
| Payment details | Surcharge amount | The total dollar amount of any surcharges applied to the claim. |
| Payment details | Surcharge % | The surcharge percentage applied to the claim. |
| Payment details | Adjudication date | The date the adjudication of the claim was completed. |
| Payment details | Check or EFT number | The check or Electronic Funds Transfer (EFT) number associated with the payment. |
| Payment details | Member penalty amount | The dollar amount of any penalty due from the member. |
| Payment details | Coinsurance amount | The total coinsurance amount due from the member. |
| Payment details | Copay amount | The total copay amount due from the member. |
| Payment details | Deductible amount | The total deductible amount due from the member. |
| Payment details | Additional liability amount | Captures any additional member liability for the services billed on the claim. |
| Payment details | LPI amount | The amount of late payment interest paid. |
| Payment details | LPI number of days | The number of days used to calculate late payment interest. |
| Payment details | LPI decisioning | The LPI decisioning hyperlink opens the decision table used to calculate late payment interest. |
| Payment details | Allowed amount | The final amount payable for the claim. |
| Payment details | Total patient estimated liability | Professional and inpatient claims only - The estimate of the patient's liability submitted by the provider. |
| Payment details | Patient liability amount | The total patient liability for the services submitted on the claim. |
| Payment details | Final paid amount | The total amount paid for the claim. |
| Payment details | Paid date | The date payment was issued for the claim. |
| Payment details | Network code | The code indicating the network. |
| Payment details | Info from external system | The Info from external system hyperlink provides access to information from external systems (for example, ClaimsXten or NetworX Pricer) used in the claim adjudication. |
| Payment details | Adjustment group code | The adjustment group code used to indicate liability for non-paid amounts on the claim. |
| Payment details | Reason code | The reason code used to explain non-paid amounts on the claim. |
| Payment details | Description | The description associated with the reason code used to explain non-paid amounts on the claim. |
| Payment details | Amount | The amount of the claim adjustment. |
| Payment details | Quantity | The quantity associated with the claim adjustment. |
| Payment details | Remittance advice remark code | The code used to further explain the adjustment to the claim. |
| Payment details | Description | The description associated with the remittance advice code on the claim. |
| Payment details | Network | The network name. |
| Payment details | OOP total | The out of pocket (OOP) total for the network. |
| Payment details | OOP yearly max | The out of pocket (OOP) yearly maximum defined for the network. |
| Section | Field name | Description |
| Case details | Last updated by | The name and timeframe of the last update made to the claim. |
| Case details | Created by | The name and timeframe of the creation of the claim. |
| Case details | Tags | Allows you to choose an existing tag or create a new one(s) in order to tag the claim work object. |
The Attachments slot provides the ability to add, delete or download attachments, based on the user role and privileges.
Previous topic Exchanging data with external systems
